Low back pain (LBP) has become the leading cause of disability world-wide. In Canada, chronic LBP (3-6 months) is ranked among the top reasons for physician visits by people less than 60 years of age. A wide range of prevalence is reported in the literature, but it is estimated that up to 84% of people will experience at least oneepisode of LBP in their lifetime. In addition, LBP is experienced by people of different cultures and of low, medium and high socioeconomic status. These statistics are alarming because there are no clear and concise guidelines for recognition, prevention and management of LBP.
If you are interested in my story, as it pertains to LBP, then please read Ramblings of a Coherent Brain #1-8. Here is a quick summary. I had my second L5 partial discectomy and S1 nerve root decompression surgery on October 29th, 2018. This second episode of LBP began from no apparent traumatic injury and, because it occurred at the previous surgical site, my surgeon believes it occurred spontaneously. This was a known complication of having the surgery the first time. Regardless of cause or current situation I find myself off work; rehabilitating from my second back surgery before the age of 30. Statistically speaking I am a member of a small sample size. No matter though, I am working to recover and prevent future episodes. As a physiotherapist I feel empowered to share my story and the current knowledge of how we treat LBP.
I believe physiotherapy is at the frontier of critically thinking about how we treat LBP. We are moving away from the fear of instability and demand of continual core engagement, to the teaching of optimal physiological movement. In the debate over the importance of specific core exercises for LBP, I believe, as others, that it is an issue with muscle activation and improper lifting techniques. Many episodes of acute LBP (< 3 months) can be avoided with regular physical activity, to keep the muscles of the spine healthy, and movement education to teach proper lifting biomechanics. I am sure you have heard about the “core muscles” before. If not, no worries, I am about to teach you. The core muscles in our body help control the lumbopelvic region, which is our pelvis and lumbar spine. The literature supports that the core muscles are the: diaphragm, pelvic floor group of muscles, deep stabilizers (multifidi), transversus abdominus (TA) and quadratus lumborum (QL). Major muscle groups (global movers) such as the latissimus dorsi (lats), erector spinae, gluteus maximus and medius, rectus abdominus, abdominal obliques and hamstrings all have attachments to the pelvis and influence the lumbar spine. The hip flexors are another major muscle group that runs from the front side of the lumbar spine and pelvis to the femur (thigh bone). What does this all mean? Changes in core muscle strength and endurance, and altered angles of force from global movers can place great stress on the lumbar spine. The core muscles act to support the lumbar spine, as the global movers produce complex movement (ex. lifting, running, throwing). The TA and lats feed into a strong layer of fascia known as the thoracolumbar fascia (anatomical back belt).
Conscious BREATHING uses the diaphragm to increase abdominal pressure and is enough to activate the TA, multifidi and pelvic floor. The TA and lats transmit forces from the upper to lower body through the thoracolumbar fascia, providing spinal stabilization. The lumbopelvic region is caught in the middle and this is where core exercise are focused. Specific core stability exercises became popular after research showed that the multifidi in people suffering from LBP were atrophied (decreased in size). QUESTION: Did the multifidi atrophy causing decreased dynamic core stabilization and LBP? OR. Did the LBP stop normal movement and cause the multifidi to atrophy from decreased core activation and disuse. Does it matter?? I don’t think so.By restoring normal physiological movement, with normal breath, individuals will activate their core, and the strength and endurance of the core muscles will improve. Remember, I am not perfect and this stiff is not easy. I have “worked on my core” for years and have had 2 back surgeries. It’s an ongoing experiment (good thing I love what I do for a living).
Why is it so hard to restore normal movement patterns during and after LBP episodes?
Humans evolved from moving and weight bearing on all four limbs. Over time we became bipedal – walking and weight bearing mostly on our legs. This was when we were mostly hunter and gathers, so movement was commonplace. Walking on all fours would have forced our abdominal and lower back muscles to constantly fire and work in order to combat gravity. Upright walking caused the forces on our spines to change, and the activation load on our core lessened. Fast forward past the agricultural, industrial and scientific revolutions and we are met with a silent foe.
SITTING. Sitting is something that requires little effort but results in increased stress on our spine and the intervertebral discs. Practicing good sitting posture and using an ergonomic chair can limit the negative effects of prolonged sitting (> 30 minutes). My burning question is … How can we “beat” sitting if it is something that is inevitably a large part of our lives? We sit to drive/transit to work where most of us sit; then we sit to drive/transit home where we sit to relax, eat and entertain ourselves. Instead of thinking of sitting as the enemy, let’s re-think the importance of movement. There is an abundance of excellent research to support exercising for optimal health (musculoskeletal, cardiovascular and mental). Simply walking engages our core and is beneficial at 30 minutes a day. This brings us back to question of why we focus on specific core exercisesfor LBP? Well, LBP, like any pain, is going to be unique to the individual. EXAMPLE: My back pain is different from my wife’s. And the specific, nuanced, core exercises that exist work from a very low level (beginner) to more advanced. The low level exercises focus on simple movement with continuous breath, while focusing attention to the abdominal and lower back muscles. This is incredibly important in the presence of pain.
I will use surgery, and specifically my surgery, as an example.
After any surgery there is pain. A major part of post-operative (post-op) care is pain management, so mobilizing (movement) can begin. I spent one night in the hospital and my instructions were to ask for pain medication, when needed, and to get up and walk as soon as I could. Unlike a hip or knee replacement, there is no post-op protocol for a partial discectomy. The research indicates that getting back to normal activities as soon as possible is best. My discharge instructions, from my surgeon, were this: 1. Return to normal activities as soon as pain permits, 2. Avoid prolonged sitting, 3. No lifting with twisting, 4. Avoid lifting things out in front of my body and keep lifted objects close, 5. Move a little more each day and 6. Follow-up with my surgeon in 4 weeks. Basically, this is what physiotherapists use as education for any back injury, besides the surgeon follow-up part. Sounds easy. HOWEVER, my ramblings from my blog series share the realities of pain management and my unique experiences that shaped how I move and think today. In the hospital I relied heavily on my experience with breathing techniques to calm my nervous system and facilitate pain control so I could begin moving the same day as my surgery.
Below is my “Beginner Guideline for Back Injury Rehabilitation”. This guideline is meant to be safe for anyone suffering from LBP and can be started immediately. Having said that, I do recommend seeing a physiotherapist if you are suffering from LBP because everyone would benefit from a thorough assessment and an experienced eye when performing exercises for the first time.
Before reading my guideline, please watch this short video by a well known Canadian physiotherapist, Dr. Bahram Jam.
https://www.youtube.com/watch?v=Gj7FoKkiamY&feature=youtu.be
I agree with Bahram. However, my personal history with pain originating from my back has made me more empathetic. It is OKAY to be tentative when experiencing or recovering from an episode of LBP. The key message from the video is to NOT be fearful of movement.
Beginner Guideline for Back Injury Rehabilitation
*This guide can be followed daily as YOUR pain permits. Any increasein pain to your back or leg(s) indicates that you should go back to #1 until your pain settles and seek further help from a physiotherapist*
- SAFE PLACE: Find YOUR position of comfort – laying flat on your back or stomach, or laying on you back with your knees up. Begin breathing in through your nose to a count of 4 seconds and out through mouth to a count of 6 seconds. Repeat this 5 times f0r 3-5 sets or 3 minutes, and use this as your warm-up/rest/recovery exercise. This will help with pain as focused breathing can calm your nervous system.
- MARCHING: Transition to laying on your back with your knees up (crook lying) and KEEP breathing, but you can stop counting. March your legs one at a time for 10 repetitions per side and repeat for 3 sets. Try to maintain a gentle contact between your lower back and the ground.
- TABLE TOP: Slowly roll onto one side and make your way into a table top (crawling position). Have your hands directly under your shoulders and knees directly under your hips. From here many exercises can be performed, BUT we will keep it simple and start with flexion and extension of your spine. If you have done yoga before, this is cat-cow. Slowly arch your back as far as you can, then round your back as far as you can. 10 times each direction for 3 sets. BREATHE. It can be beneficial to time your inhale with extension (cow) and your exhale with flexion (cat).
- CRAWL: If all is going well, crawl forward for 5-10 steps and then crawl backwards for 5-10 steps. Repeat for 3 sets. Don’t think too much, just move with your breath.
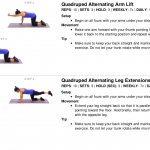
- TABLE TOP ARM/LEG LIFTS: Return to the table top position and focus on having equal weight on both hands and knees. Lift one arm at a time, then one leg at a time and repeat this for 3 sets of 10. As one arm/leg is lifted you will feel your spine want to twist. Keep your back flat and try to keep equal weight on the remaining 3 points of contact with the ground.
- WALK: Finally, slowly make your way into standing and walk. The goal is to accumulate 30 minutes a day. This can be broken in small increments such as 6 sets of 5 minutes or 3 sets of 10 minutes. What matters is trying to meet that 30 minute goal, daily.
Follow this URL: https://www.medbridgego.com/and enter the CODE: 4RPLVLBXto get access to an online program that has pictures and instructions for the above exercises.
Thanks for reading!
David Ridgewell MPT, BSc Kin, CAFCI, IMS
References:
Akuthota, V, Nadler, S.F. (2004). Core strengthening. Archives of Physical Medicine and Rehabilitation. Vol. 85, supplement 1, pages 86-92. DOI: https://doi.org/10.1053/j.apmr.2003.12.005
Lacasse, A et al. (2017). The Canadian minimum dataset for chronic low back pain research: a cross-cultural adaptation of the National Institutes of Health Task Force Research Standards. camjOPEN.Vol. 5, no. 1, E237-248. DOI: 10.9778/cmajo.20160117
Hartvigsen, J. (2018). What low back pain is and why we need to pay attention. The Lancet.Vol. 391, issue 0137, pages 2356-2367. DOI: https://doi.org/10.1016/S0140-6736(18)30480-X
LBP video: Bahram Jam, PT. Advanced Physical Therapy Education Institute.