Many of us have experienced the impacts of Osteoarthritis (OA) whether that be in ourselves or our friends and family. As a physiotherapist working with people struggling with OA, I am often struck by the confusing messages and misinformation around OA. I hope this post will provide some myth busting and leave you informed about the current evidence, treatment and emerging prevention strategies.
.
First, let’s look at some of the data. From a 2021 special report on Osteoarthritis (OA) commissioned by the Arthritis Society [1], we gain insight on OA in Canada:
-
- About 15% of Canadians 20 years and older have OA = 4 million or 1 in 7 Canadians
- More than 52% of those with OA are under 65 years old and 1/3 are under 25
- More than 90% of people with OA have joint pain, stiffness or aching
- The knee is the most common symptomatic joint
- More women than men are impacted
- 2/3 of people with OA report decreased sleep quality
- Those with OA are more likely to be diagnosed with a mood or anxiety disorder reminding us of the interplay between pain, function and mood
- Younger adults with OA report greater life dissatisfaction compared to older adults with OA or the general population
Now that we have that background, how about a little True or False to help us understand OA a little better?
1) Osteoarthritis is the most common reason for inactivity as people age.
TRUE! Often this is due to a lack of understanding of OA and chronic pain.
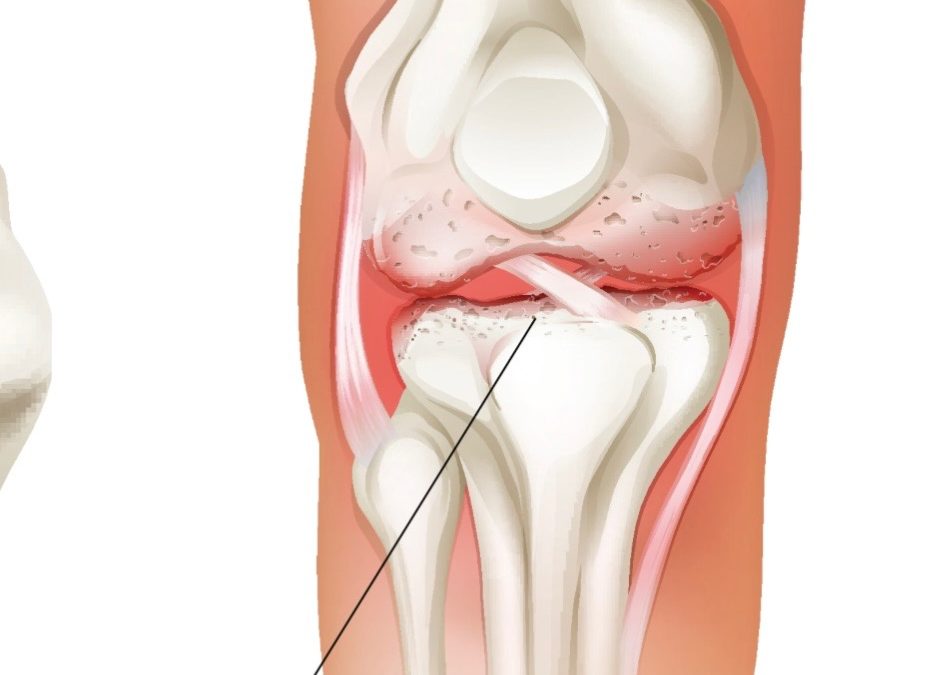
2) Osteoarthritis is a wear and tear disease.
FALSE! Osteoarthritis is a disease that affects the whole joint from an imbalance in the normal regeneration/degeneration cycle of cartilage in the joint.[1] The cartilage needs moderate loading and unloading to keep the joint healthy and happy.
3) Osteoarthritis means I have bone on bone in my knee and that’s what causes my pain.
FALSE! It’s impossible to have “bone on bone” because despite changes in cartilage and bone with OA, we also have fluid in these spaces.
4) I have to get an X-ray to know if I have OA in my knee.
FALSE! An X-ray is not necessary to diagnose OA. OA is diagnosed through a combination of pain/symptoms, risk factors and clinical examination by your physiotherapist. Symptoms guide the choice of treatment, not the X-ray as we know that some people have OA on X-ray but no limiting pain or symptoms.
5) There’s nothing I can do about my knee OA.
FALSE! There are many modifiable risk factors such as muscle weakness, physical inactivity, obesity and joint injury or overload. Working on building up your toolbox of “self-management” treatments to reduce the impact of OA on your life is invaluable to decrease pain, return to activities and delay surgery. Research tells us that everyone with OA can benefit from adding education, exercise and weight management to their routines. Some people will need pharmacological pain relief and treatments from a physiotherapist. And there will be a few who progress to surgery but surgery is no longer the first ‘go-to’ it once was. Your CAMPT-certified physiotherapist will help you build this toolbox.
6) The surgeon told me I need a knee replacement so I’ll just have to wait until my surgery to feel better.
FALSE! It may be that you are at a point where you need a joint replacement. While you wait, you can work on all the modifiable factors including pain, weight, overload, strength and activity levels.
7) My doctor told me I need to lose weight.
TRUE! And…There is a growing body of evidence that suggests that with obesity there is an inflammatory component and changes in the immune system that contribute to OA, possibly more than the loading from weight alone. [3]
8) I’ve heard that I can work on retraining my brain and nervous system so that my pain is more under control.
TRUE! Pain is a complex experience and we know that over time, some people with chronic OA pain find their joints and other areas of the body can become sensitive and even hyper-sensitive. To learn more about chronic or persistent pain and how to help change your pain, please watch this video https://www.tamethebeast.org/#tame-the-beast
9) I had a traumatic injury to my knee skiing so I’ll have more OA in my knee.
FALSE! In 2022, a Canadian physiotherapist/researcher and colleagues published the ‘OPTIKNEE’ consensus on optimising knee health after traumatic knee injury to prevent OA.[4],[5] Among the recommendations for preventing OA progression are monitoring for: pain and symptoms; muscle strength in quads and hamstrings; functional performance such as a single hop test after a traumatic knee injury.
10) It is dangerous to run now that I have knee OA.
False and True…it depends! We know that many people with knee OA do not have symptoms or limitations and we know that part of keeping our knees healthy is a normal cycle of load/unload to keep the degeneration/regeneration cycle in the cartilage. Reviews of the research find that there is wide variety in the quantity and quality of knee OA and more importantly whether or not this correlates with pain or decreased function is variable.. If you aren’t sure whether running is okay for you, ask your physiotherapist.
I hope your understanding of knee OA has grown. Please remember the following:
1)You do not need an xray to diagnose OA
2)OA is common and not necessarily related to older age
3)After a traumatic knee injury, you can work on preventing OA progression
4)Everyone with OA can benefit from education, exercise and weight management
If you or someone you know is suffering with knee OA or you are recovering from an acute knee injury and want to work on prevention, see your CAMPT certified physiotherapist for guidance.
Diane Roylance, PT BSc(Zool), BScPT, FCAMPT, cGunn IMS
Resources:
Running and knee OA:
https://www.jospt.org/doi/pdf/10.2519/jospt.2017.0505
https://bjsm.bmj.com/content/56/6/357
https://msklab.med.ubc.ca/optiknee/
CAMPT certified Physiotherapists:
[1] Special Report: The Burden of OA in Canada (2021). Badley EM et al.
[2] GLA:D Canada (2023)
[3] Sakkas et al. The Role of T cells in the pathogenesis of OA. Arthr Rheumatol 2007 56 (2): 409-24.
[4] Whittaker JL et al. Risk factors for knee osteoarthritis after traumatic knee injury: a systematic review and meta-analysis of randomised controlled trials and cohort studies for the OPTIKNEE Consensus. BJSM 2022 Vol.56, issue 24.
[5] https://msklab.med.ubc.ca/optiknee/
[6] https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-9-116